Adoption of Anesthesia Information Management Systems (AIMS) continues to accelerate. It is estimated that 75% of US academic anesthesiology departments are using an AIMS and that this will rise to 84% by 2020.1 Within a few short years, it is likely that residents finishing training will have no significant experience charting on paper. AIMS are well poised to become the standard of care for anesthesia documentation.
Adoption has been facilitated by numerous promises, many of which have been discussed in previous APSF Newsletters.2 These include, but are not limited to improved legibility, more accurate data capture, improved chart completion, real-time decision support, more complete charge capture, new opportunities for clinical research, better quality improvement data, and participation in quality outcomes registries.
Multiple studies in the literature support these benefits, though many of these advantages have also been dependent on significant customization or homegrown systems. Customization is necessary because the standard out-of-the-box functionality for many of the popular systems fail to achieve even the most basic of benefits. The literature also suggests the need for substantial financial resources and dedicated staff to support both the implementation and maintenance of an AIMS. As health care dollars become more scarce, this promises to become increasingly challenging. What follows is a review of some of the claims outlined above and a discussion of the current state of AIMS.
Legibility
AIMS have matured anesthesia care documentation from illegible scribble to organized data with clear graphics (Figure 1). It is no longer necessary to decipher another clinician’s handwriting when reviewing an anesthetic record or to squeeze comments sideways into the margin to ensure one’s thoughts are completely documented.
This advance is not without tradeoffs. A typical 3-hour paper anesthetic record contains 264 data points.3 In contrast, the same record documented on an AIMS may contain more than 10 times as many data points. Not only do AIMS automatically capture the patient’s physiologic and respiratory data with greater fidelity, they frequently require clinicians to manually document substantially more information as well.
Thus, a typical anesthetic no longer fits concisely on a single sheet of paper. It is now necessary to review multiple printed pages or scroll through dozens of screens to view a record in its entirety. These new records are perfectly legible, but often difficult to follow.
Chart completion
There are many studies on chart completion with AIMS. Despite the belief that AIMS automatically improve chart completion, these studies show mixed results. Edwards et al. demonstrated a significant improvement in 6 data elements with the implementation of an AIMS.4 Shear et al. reviewed 200 paper records prior to AIMS implementation and 200 records after AIMS implementation. The study evaluated 17 data elements, finding that completion of 7 elements declined and only 1 improved with AIMS implementation. A subsequent evaluation was completed at 7 and 15 months, finding improvement in all deficiencies, yet at levels still inferior to paper charting.3 This improvement was related to the addition of customized hard stops before record closure, and it emphasizes the opportunity for human factor engineers to further optimize AIMS.
Nevertheless, there is promise. Sandberg et al., looked at allergy documentation in the electronic anesthesia record. At baseline, he found that 30% of charts were missing basic allergy documentation. A customized system was developed to page the anesthesia provider if allergies were not documented within 15 minutes of the anesthesia start time. Following implementation, the missing allergy documentation rate fell to 8%.5 Similarly, a recent review of AIMS data by McCarty et al. demonstrated the ability to improve chart completion. In their study, complete airway documentation improved from 13.2% to 91.6% by using an AIMS in conjunction with deliberate process improvement tools and integrated decision support.6
While there is tremendous potential, most chart completion benefits to date have required a homegrown IT solution, locally focused process improvement efforts, and significant financial and clinical resources.
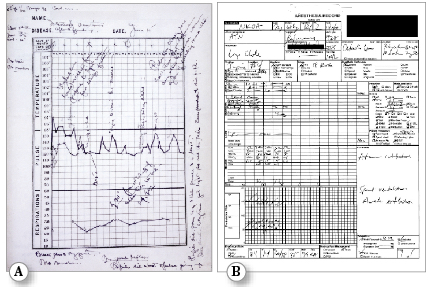

Figure 1: a) The original Harvey Cushing Ether Chart from 1895 courtesy of Massachusetts General Hospital Archives and Special Collections b) Modern paper anesthesia record c) Electronic anesthesia record
Better Quality Data
AIMS promise to supply us with more accurate and more plentiful quality data. Peterfreund et al. developed a secure electronic system to capture quality assurance information linked to an automated anesthesia record.7 They nearly doubled the number of quality assurance events captured by instituting a hard stop in their AIMS. In addition, the ease of reporting was improved by seamlessly linking the process of quality reporting with case documentation.
In contrast to the improvement shown by Peterfeund et al., the results reported by Pruitt et al. at Children’s Hospital of Philadelphia show continued cause for concern. They retrospectively reviewed AIMS and Continuous Quality Improvement (CQI) reports of 995 pediatric patients.8 Observers recorded 8 cases of emesis during induction and all were confirmed with the attending anesthesiologist. However, only 3 were recorded in AIMS records and only 1 was documented in the CQI. While no comparison was made to paper records in this study, it highlights the ongoing challenge to capture manually documented events, even with an AIMS.6
Another significant promise is the use of registry data to provide an evidence-based foundation for guiding treatment. By compiling large quantities of data from a diverse group of institutions, it may be possible to identify hidden trends and draw conclusions in new and unique ways. However, it is necessary to remain cognizant of the concept that “garbage in = garbage out.” There is often a misguided belief that conclusions drawn from database mining are more accurate. In fact, the quality of this data is poorly understood. In order to truly have comparable quality data, standard data definitions are needed. Groups like the Multicenter Perioperative Outcomes Group (MPOG), the Anesthesia Quality Institute (AQI) and the APSF are currently working to define those terminologies.9 Until their work is complete, one must read any conclusions with a cautious eye.
Distraction
AIMS have added new complexities to our already chaotic work environments. What used to fit on one side of an 8 ½” x 11” sheet of paper is now buried beneath dozens of screens. Depending on comfort with computers and experience with these systems, there is a very significant potential for distracting a clinician from our primary mission: vigilant patient care.
The distraction risk has been well studied, demonstrating that those who are distracted perform at a level similar to being sleep deprived or intoxicated. One need only observe a car swerving in front of them to realize the dangerous effects of distraction on performance. Indeed, AAA found that as mental workload increases, reaction time slows, brain function is compromised, drivers scan the road less and often miss otherwise obvious visual cues.10 Though not well studied in the anesthesia literature, it must be assumed that our providers are equally susceptible to these effects.
Discussion
Many of the benefits achieved with AIMS require additional custom programming to bring to fruition. Moving forward, we will need to continue to push the AIMS vendors to incorporate user friendly and meaningful decision support capabilities into their systems. As you embark on your AIMS journey, we encourage you to follow the path outlined in the literature. You will need a clinical champion who understands your institution’s anesthesia workflow and the inner workings of your AIMS functionality. You should seek non-clinical support to help manage, maintain, and troubleshoot any issues as they arise. In many ways, the biomedical team has become equally important as the anesthesia providers in the world of the AIMS.11,12
There is no doubt that AIMS are here to stay. They offer a powerful set of tools that promise to improve the care we provide. However, these systems are far from mature and they continue to have significant limitations. We need to be cognizant of their shortcomings, and redouble our efforts to remain vigilant. After all, next to every AIMS lies someone’s loved one.
Mark A. Deshur, MD, MBA Director of Anesthesia Information Technology Director of Pediatric Anesthesia NorthShore University HealthSystem Clinical Assistant Professor University of Chicago, Pritzker School of Medicine
Wilton C. Levine, MD Associate Medical Director Perioperative Services Massachusetts General Hospital Assistant Professor Harvard Medical School
References
- Stol IS, Ehrenfeld JM, Epstein RH. Technology diffusion of anesthesia information management systems in to academic anesthesia departments in the United States. Anesth Analg 2014;118:644-50.
- Thys DM. The role of information systems in anesthesia. APSF Newsletter 2001;16:3
- Shear TS, Mitchell JS, Deshur MA. The effect of anesthesia charting modalities on the rate of charting deficiencies: A comparison of paper and electronic anesthesia records. ASA Abstract, 2013.
- Edwards KE, Hagen SM, Hannam J, Kruger C, Yu R, Merry AF. A randomized comparison between records made with an anesthesia information management system and by hand, and evaluation of the Hawthorne effect. Can J Anaesth 2013;60:990-7.
- Sandberg WS, Sandberg EH, Seim AR, Anupama S, Ehrenfeld JM, Spring SF, Walsh JL. Real-time checking of electronic anesthesia records for documentation errors and automatically text messaging clinicians improves quality of documentation. Anesth Analg 2008;106:192-201.
- Mccarty LK, Saddawi-Konefka D, Gargan LM, Driscoll WD, Walsh JL, Peterfreund, RA. Application of process improvement principles to increase frequency of complete airway management documentation. Anesthesiology 2014;121:1166-74.
- Peterfreund RA, Driscoll WD, Walsh JL, Subramanian A, Anupama S, et al. Evaluation of a mandatory quality assurance data capture in anesthesia: A secure electronic system to capture quality assurance information linked to an automated anesthesia record. Anesth Analg 2011; 112(5):1218-25.
- Pruitt EY, Simpao A, Cook-Sather S, Rehman M. Reliability of critical event reporting in an Anesthesia Information Management System (AIMS). Society for Technology in Anesthesia (STA) Annual Meeting Abstract #54. 2012.
- Monk TG, Hurrell M, Norton A. Anesthesia Information Management Systems: Toward standardization of terminology in Anesthesia Information Management Systems. APSF Newsletter. https://dev2.apsf.org/initiatives_systems.php. Accessed May 1, 2015.
- Strayer et al. Cognitive distraction in the vehicle, AAA Foundation for Traffic Safety, 2013. Human Factors Summer 2006;48(2):381–391.
- Sandberg WS. Anesthesia Information Management Systems: Almost There. Anesth Analg 2008;107:1100-02.
- Ehrenfeld JM. Anesthesia Information Management Systems: A guide to their successful installation and use. Anesthesiology News, September, 2009.


 Issue PDF
Issue PDF