Dear Rapid Response:
Introduction
For maxillofacial fracture repairs, surgeons often prefer nasal intubation to allow for intermaxillary fixation. However, there are circumstances when nasal intubation is contraindicated, such as Lefort II and III, in which fractures to the ethmoid bone often extend to its cribiform plate 1. In these situations, other airway techniques, such as tracheostomy or submental intubation, should be considered 2.
Tracheostomy is a reliable approach to securing an airway and allows for long-term ventilatory support; however, there is significant morbidity associated with these procedures. Complications include hemorrhage, infection, and tracheal stenosis with morbidity rates of 15.8% and mortality rates of 1.6% 3, 4, 5. Thus, the risks of tracheostomy may outweigh the benefits in patients not requiring postoperative ventilatory support.
There have been studies of submental intubation, proposing it as a safe alternative to tracheostomy for some patients. Given the curved trajectory that the endotracheal tube (ETT) takes to reach the submental location, studies recommend a flexible, kink resistant tube with a detachable connector 2. However, published case reports have noted the increased rarity and cost in finding kink resistant tubes with detachable connectors 6.
Some reports have proposed manually detaching a reinforced ETT from the universal connector to loosen the binding with subsequent reattachment for use in the case 6. We present a case of submandibular intubation that used this technique for intubation with resulting obstruction of the tube lumen by a plastic binding material that comprised the armored tube.
Case Summary/Discussion
The patient is a 35 year-old man who presented with multiple facial fractures after being assaulted. Injuries included bilateral Le Fort fractures and right nasoorbitoethmoid fracture (Markowitz type I). Facial CT demonstrated fracture to cribriform plate and outer table of frontal sinus. CT brain was negative for intracranial blood or pneumocephalus. No clear rhinorrhea was appreciated. The patient was emergently brought to the operating room for open reduction internal fixation of complex maxillofacial fractures with a plan for submental intubation.
Patient underwent routine induction and oral intubation with an armored ETT (Teleflex Rüsch® Flex Endotracheal Tube, Ref 103902070). Intubation was performed via Altemir sequence: the ETT was detached from the universal connector and exteriorized via submental dissection 6. Difficulty was noted when separating the endotracheal tube connector from the ETT due to the plastic binding adhering the two pieces together. The remainder of the case continued without issue.
Upon completion of surgery, the patient was given sugammadex with quantitative train of four (TOF) > 90 and respiratory rate of 8-10 with tidal volumes > 400 cc. The ETT was relocated back to the oropharynx with the ETT connector detached during this relocation.
As the patient progressed towards emergence, there was a decrease in tidal volumes with increased hypercapnia. Narcotic overdose was considered, however low tidal volumes with appropriate respiratory rate made this less likely. An additional 200 mg sugammadex given for possible muscle weakness, but adequate reversal (TOF = 100) was appreciated on repeat quantitative assessment. After these interventions, there was concern for airway obstruction and differential diagnosis included endobronchial intubation, bronchospasm, kinked endotracheal tube (ETT), kinked breathing circuits, and foreign body. Tube depth was evaluated and bilateral chest rise was appreciated, however tidal volumes remained low. We maintained anesthesia with intermittent propofol boluses. Neither a kink in the tube nor circuit was appreciated during visual assessment. The decision was made to keep the patient intubated and admit to ICU for further evaluation. Because of our institutional preference of using standard ETTs for ICU patients, we prepared for an ETT exchange.
We initially experienced difficulty passing the exchange catheter. On exam, it was noted that a piece of adhesive remnant from the armored tube had obstructed the lumen (Figure 1). The piece was removed with mosquito clamps and the tube was then easily exchanged for a standard 7.5 ETT without additional complications. ETCO2 and tidal volumes subsequently improved.
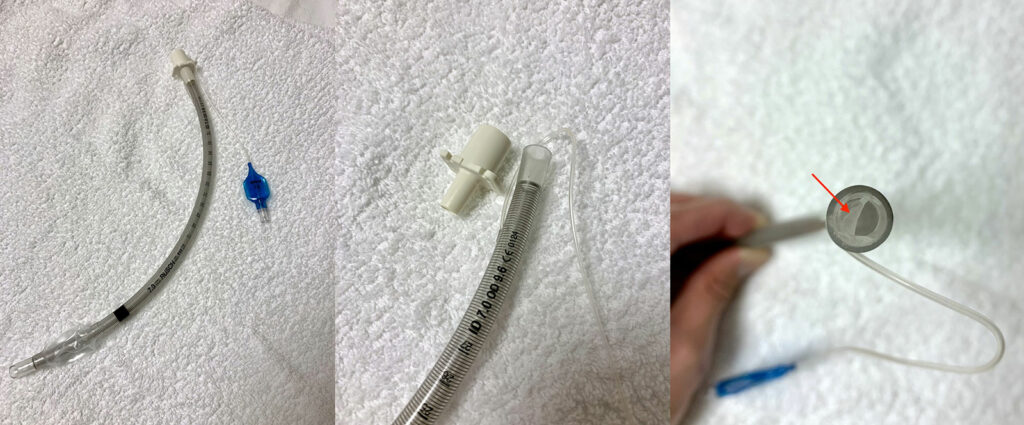
Figure 1: Armored endotracheal tube with universal connector detached revealing adhesive remnant, previously used to bind universal connector to endotracheal tube
Conclusion
Submental intubation was originally proposed in the 1980s as a practical approach to airway management of complex maxillofacial fractures requiring only an armored tube with detachable universal connector. However, the armored tubes used in the 1980s had detachable connectors, which is no longer ubiquitous. Since then, there have been reports proposing the use of armored ETTs without detachable connectors, but our report details a situation where this approach may be a safety issue.
In reflecting upon the process and outcome of this case, we considered the use of a tube exchanger for the Altemir sequence followed by an endotracheal tube placement over the catheter. The benefit of this approach is that these catheters typically feature an easily detachable connector, however this method has not been validated in the literature. Another solution we propose is careful removal of the connector from the armored endotracheal tube with vigilant inspection of the lumen prior to patient intubation and frequent reassessment of the tube during the surgery. However, we would be cautious about selecting this approach should the patient have a tenuous airway and would consider a tracheostomy as a safer and more reliable alternative, keeping in mind that tracheostomies are also not without complications as well.
Although the authors recognize the benefits of submental intubation, we hope that our experiences help illustrate a potential consideration in the practice of separating the tube from the universal connector in non-detachable armored ETTs.
Libing Wang is a resident physician in Anesthesiology at UCLA Medical Center, Los Angeles, CA, USA
Jason Pia is a resident physician in Anesthesiology at UCLA Medical Center, Los Angeles, CA, USA
Emily Methangkool is an associate clinical professor and vice chair for quality and safety in Anesthesiology at UCLA Medical Center, Los Angeles, CA, USA
Jason Yu is an assistant clinical professor in Oral & Maxillofacial Surgery at UCLA Medical Center and UCLA School of Dentistry, Los Angeles, CA, USA
Carsten Nadjat-Haiem is a clinical professor in Anesthesiology at UCLA Medical Center, Los Angeles, CA, USA
None of the authors have any conflicts of interest.
References
- Chauhan V, Acharya G. Nasal intubation: A comprehensive review. Indian J Crit Care Med. 2016;20(11):662-667. doi:10.4103/0972-5229.194013
- Jundt JS, Cattano D, Hagberg CA, Wilson JW. Submental intubation: a literature review. Int J Oral Maxillofac Surg 2012;41:46-54.
- Chew JY, Cantrell RW. Tracheostomy: Complications and Their Management. Arch Otolaryngol. 1972;96(6):538–545. doi:10.1001/archotol.1972.00770090816008
- Durbin CG Jr. Tracheostomy: why, when, and how? Respir Care. 2010 Aug;55(8):1056-68. PMID: 20667153.
- Corbett HJ, Mann KS, Mitra I, Jesudason EC, Losty PD, Clarke RW. Tracheostomy–a 10-year experience from a UK pediatric surgical center. J Pediatr Surg. 2007 Jul;42(7):1251-4. doi: 10.1016/j.jpedsurg.2007.02.017. PMID: 17618889.
- Youn GH, Ryu SY, Oh H, et. al. Endotracheal Intubation Using Submandibular Approach for Maxillofacial Trauma Patients: Report of 2 Cases. Journal of the Korean Dental Society of Anesthesiology. 2014;14. 227. 10.17245/jkdsa.2014.14.4.227.
- Hernández Altemir F. The submental route for endotracheal intubation. A new technique. J Maxillofac Surg. 1986 Feb;14(1):64-5. doi: 10.1016/s0301-0503(86)80261-2. PMID: 3456416.
In Response:
Thank you for the opportunity to comment on the rationale for the design of the connector on the Rüsch Flex Endotracheal tube.
These endotracheal tubes are indicated for oral and nasal intubation for airway management in the care of patients in whom there is an increased risk of the tracheal tube being blocked by kinking when the head and neck are in extreme positions. To our knowledge, there are no airway devices specifically indicated for use in the Altemir Sequence, since this calls for first conventional orotracheal intubation followed by the exteriorizing of said oral endotracheal tube through the floor of the mouth and submental triangle 1. This was for the express purpose of avoiding tracheostomy and allowing for the concomitant restoration of occlusion and reduction of facial fractures in patients ineligible for nasotracheal intubation.
Due to the nature of the manufacture of these reinforced endotracheal tubes, destructive disassembly will damage the device, running the risk of obstructing the lumen when used in this off-label manner and, as a manufacturer, would advise against such off-label use. We do, however, manufacture a reinforced endotracheal tube whose 15mm connector is designed to be detached and reattached for the indication of fibreoptic intubation. Nonetheless, use of even this device in the Altemir Sequence would still be off-label. It is worth noting that the literature does describe damage to endotracheal tubes during this procedure 2.
Sincerely yours,
Dr Stephen Luney MB, BCh, BAO, FFARCSI
Medical & Safety Director, Clinical & Medical Affairs
Teleflex
References
- Altemir FH, Montero SH, Hernández Montero S, Hernández Montero E, Moros Peña M. Hazards of submental tracheal intubation. Anaesthesia 2004;59:1140.
- S Jundt, et al. Submental intubation: a literature review Int. J. Oral Maxillofac. Surg. 2012; 41: 46–54

 Articles
Articles