Introduction
Many of the technological advancements adopted by our specialty such as the pulse oximeter, capnography, brain function monitoring, and video laryngoscopy have revolutionized patient care and safety and have been adopted by other clinicians involved in acute care. In the recent past, there was heated debate, including in this Newsletter,1 regarding the impact of ultrasound in increasing patient safety for the placement of central lines and nerve blocks. Similarly, we believe that Portable Point of Care Ultrasound (PPOCUS) which involves the use of handheld, portable, affordable, easy-to-use ultrasound devices to perform point of care ultrasound (POCUS) is an emerging technology that has the potential to improve perioperative patient safety.
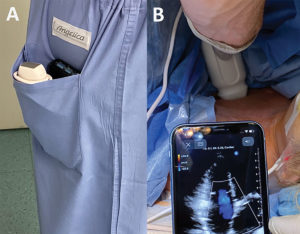
Figure 1: Extreme portability afforded by portable ultrasound devices (Panel A) and use of PPOCUS in perioperative settings such as in the operating room (Panel B).
PPOCUS is undergoing a revolution similar to what computing technology experienced in the 20th century, an acceleration in the development of portable, efficient, and affordable systems. Ultrasound technology has evolved to the point that portable ultrasound devices can now fit seamlessly in a clinician’s back scrub pocket (Figure 1) at a price point as low as $2000 USD. Furthermore, the imaging capabilities far exceed many of the best ultrasound machines of decades ago.
The revolution in PPOCUS is facilitated not just by the portable nature of the hardware of current pocket-sized ultrasound devices, but also by the software available to support the user and its adoption. Many of the conventional ultrasound devices require rudimentary methods such as USB cables to download and store images. However, the newer PPOCUS devices are now able to directly upload acquired images to the cloud via WiFi or cellular network. This new technological capability can seamlessly be integrated into the Picture and Archiving Communication System (PACS) and patient’s electronic medical record system. PPOCUS studies are able to be de-identified with a single click2 in order to maintain patient privacy and confidentiality. However, specific institutional guidelines to protect patient privacy regarding storing this information is variable throughout the US. Nevertheless, this easy integration that meets HIPAA-compliant standards allows for immediate collaboration with other health care providers as well as providing new real-time opportunities for quality assurance of the studies obtained. In addition, some of the handheld devices have novel teleguidance technologies that allow ultrasound experts to guide novice ultrasound users through an ultrasound exam remotely and allow for live image acquisition, interpretation, and feedback.3 Artificial intelligence is expected to further facilitate image acquisition and interpretation, providing real-time clinically relevant capabilities such as the determination of left ventricular function and the presence of pulmonary edema.
Indications and Limitations of PPOCUS
The increased accessibility of PPOCUS devices has allowed for its meaningful use in a variety of patient care situations where perioperative ultrasound may impact patient outcomes.4 In our practice at the Massachusetts General Hospital (MGH), we have adopted handheld ultrasound devices within all perioperative domains to make time-sensitive diagnoses, perform serial assessments, and guide important management decisions. Table 1 shows the many indications for the perioperative use of PPOCUS by anesthesia professionals. Table 2 compares PPOCUS with POCUS which highlights many of the advantages and limitations of this technology.
Table 1: Emerging Indications for PPOCUS Use by the Anesthesia Professional
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Table 2: Summary of the similarities and differences of POCUS with portable ultrasound devices (PPOCUS) compared to conventional ultrasound platforms
| Characteristic | PPOCUS | Conventional US |
| Cost | $2,000 to $12,500 | $30k to 100k+ |
| Portability/space requirements | Extreme portability/Devices can fit in a scrub pocket and many weigh less than a pound | Not always portable/Devices may weigh up to hundreds of pounds |
| Bootup time | Seconds | Up to minutes |
| Time to successful deployment and use | Quick, given extreme portability | Slow, given labor intensive to mobilize |
| Electrical outlet requirement | No | Some |
| Quality of imaging | Good enough for binary decision-making | Generally higher quality imaging |
| EKG synchronization capability | No | Yes |
| Ability to use in situations where space is limited | Yes | No |
| Transesophageal echocardiography capability | Not presently | Yes |
| Potential for disruption to ongoing critical care support (i.e., chest compressions) | Low | High |
| Wireless and/or 3G integration with the PACS | Some | Some |
| Allows for quick de-identification of studies to facilitate external collaboration | Yes | No |
| Teleguidance and AI capability to facilitate data acquisition, interpretation, and collaboration | Many | Limited |
| Knobology (or the functionality of controls on ultrasound device) | Limited, which may facilitate use by novice users | Extensive, which may complicate use |
| Ability to use M-mode and color doppler | Yes | Yes |
| Ability to use PWD, CWD, and TDI | No | Yes |
| Integration with EMR, PACS | Many | Most |
Abbreviatons: Artificial Intelligence (AI), Continuous Wave Doppler (CWD), Electronic Medical Record (EMR), Picture Archiving and Communication System (PACS), Pulse Wave Doppler (PWD), Tissue Doppler Imaging (TDI), ultrasound (US)
Facilitating Adoption and Competency for PPOCUS
Widespread adoption of a new technology like ultrasound can be daunting due to lack of familiarity, formal training, or a conditioned reliance on formal services staffed by cardiologists and cardiac anesthesiologists. Surveys of anesthesiologists have revealed the fear of missed diagnoses and the lack of formal training or certification as important barriers to the adoption of focused TTE in their practice.5 Understandably there are many who may be concerned about the medical/legal ramifications of “nonexperts” performing PPOCUS. This is a valid concern for both users and hospital administrators. However, it is reassuring that the known malpractice lawsuits to date have related not to the misdiagnosis and misinterpretation of POCUS, but rather to the entire lack or delay in the use of POCUS.6–8
At MGH, PPOCUS was initially employed by ultrasound enthusiasts who were looking to be self-reliant in evaluating and rescuing their own patients before things “spiraled out of control.” Anesthesia professionals who were PPOCUS enthusiasts increasingly began to respond to “anesthesia stats” and emergencies in a variety of clinical arenas in which we practice, and PPOCUS demonstrated its utility to others by answering clinically important questions in a rapid time frame. PPOCUS was shown to be instrumental in the rapid assessments of acute conditions, allowing patients to be rescued even before our formal rescue echo service could be fully mobilized, which helped to facilitate its adoption in the department. Further support for PPOCUS was achieved in our department after it demonstrated its utility in avoiding unnecessary transfer of patients to higher levels of care such as the ICU, resulting in better utilization of limited hospital resources with the rapid identification of reversible causes of deterioration gleaned by clinicians using it.
One of the major advantages of PPOCUS is that it can be readily used by all, without a significant amount of training. Prior studies suggest that physicians with limited prior ultrasonographic experience can gain proficiency in focused ultrasound with limited training, such as a 1-day workshop and as few as 20 practice scans.9,10 Of note, the American College of Chest Physicians (ACCP) requires 20 TTE studies to earn the certificate of completion for POCUS. The American College of Emergency Physicians (ACEP) requires a minimum of 25 studies per imaging application. Similarly, the Society of Point of Care Ultrasound recommends a minimum of 25 studies for certification in POCUS. Similar competencies might be developed for PPOCUS.
Recommendations and strategies to facilitate PPOCUS Use
Our PPOCUS philosophy is that “anyone can do it”—not just cardiac anesthesiologists and cardiologists. Our educational strategy has been to target clinicians that are interested in implementing this technology in their daily practice and subsequently champion its use throughout the department. PPOCUS is ideal for ultrasound education because the “activation energy” required to teach novice users ultrasound skills, and for novice users to practice those skills, is significantly reduced due to the extreme portability, affordability, and ease of use.
At the MGH, we have found that PPOCUS has helped to facilitate ultrasound training of over 40 anesthesia professionals over the last 6 months without requiring significant departmental support and a formalized structured training program. While we have formal training modules available, we do not initially require their use so as to avoid dissuading the learners before they’ve had enough hands-on training with an expert to develop some self-confidence and enthusiasm applying the new skill in clinical practice.
Enthusiastic novice users often find their own interesting resources (i.e., YouTube, podcasts, websites, etc.) to facilitate their self-learning, independently practice on our high fidelity TTE simulator, and perform a minimum of 5–10 studies one-on-one with an expert user until they are able to adequately perform a limited study on their own. Most achieve competence in obtaining the standard cardiopulmonary views (parasternal long axis, parasternal short axis, apical four-chamber view, subcostal four-chamber view, IVC view, and lung ultrasound) within 20 studies that are performed in a short period of time (within a month). We attempt to facilitate access to portable ultrasound devices so that learners can sustain the momentum necessary to achieve rapid growth of their POCUS skills. Interestingly, many of the clinicians most receptive to learning PPOCUS are early in their anesthesia training (i.e., CA-1). We hope that the junior anesthesia trainees will go on to train both the current and the next generation of anesthesia professionals so that our entire department will become experts in POCUS.
Conclusion
The incorporation of PPOCUS into perioperative care seems inevitable given its potential to enhance patient safety. It is therefore important to consider the optimal means of incorporating this technology into clinical practice and ensuring that it is used correctly by building appropriate training curriculums. For example, early targets for implementation might include integration into simulation training, emergency manuals, residency training programs, and perioperative domains where feasible. Our specialty, which has been a pioneer in patient safety should promote proficiency in PPOCUS similar to the field of emergency medicine over a decade ago.11,12 Anesthesia professionals should embrace and innovate its use as a new paradigm for patient safety and education in perioperative medicine.
Dr. Lindsay is a resident in the Department of Anesthesia, Critical Care, and Pain Medicine at the Massachusetts General Hospital, Boston, MA.
Dr. Gibson is a resident in the Department of Anesthesia, Critical Care, and Pain Medicine at the Massachusetts General Hospital, Boston, MA.
Dr. Bittner is an associate professor in the Department of Anesthesia, Critical Care and Pain Medicine at the Massachusetts General Hospital, Boston, MA. He is an associate editor of the APSF Newsletter.
Dr. Chang is the assistant program director of the Critical Care Anesthesiology Fellowship and a member of the faculty in the Department of Anesthesia, Critical Care and Pain Medicine at the Massachusetts General Hospital, Boston, MA.
The authors do not have any disclosures.
References
- Overdyk FJ. Ultrasound guidance should not be standard of care. APSF Newsletter. Winter 2002;17. https://dev2.apsf.org/article/ultrasound-guidance-should-not-be-standard-of-care/ Accessed December 4, 2019.
- Sharing studies. Website of the Butterfly Network. 2019.
- Blood AM, Judy R. The latest in cardiovascular hand-held point-of-care ultrasound: the power of echocardiography anytime, anywhere. Website of the American College of Cardiology: Latest in Cardiology. August 12, 2019.
- Canty DJ, Royse CF, Kilpatrick D, et al. The impact on cardiac diagnosis and mortality of focused transthoracic echocardiography in hip fracture surgery patients with increased risk of cardiac disease: a retrospective cohort study. Anaesthesia. 2012;67:1202–9.
- Conlin F, Connelly NR, Eaton MP, et al. Perioperative use of focused transthoracic cardiac ultrasound: a survey of current practice and opinion. Anesth Analg. 2017;125:1878–1882.
- Blaivas M, Pawl R. Analysis of lawsuits filed against emergency physicians for point-of-care emergency ultrasound examination performance and interpretation over a 20-year period. Am J Emerg Med. 2012;30:338–41.
- Nguyen J, Cascione M, Noori S. Analysis of lawsuits related to point-of-care ultrasonography in neonatology and pediatric subspecialties. J Perinatol. 2016;36:784–6.
- Stolz L, O’Brien KM, Miller ML, et al. A review of lawsuits related to point-of-care emergency ultrasound applications. West J Emerg Med. 2015;16:1–4.
- Cowie B, Kluger R. Evaluation of systolic murmurs using transthoracic echocardiography by anaesthetic trainees. Anaesthesia. 2011;66:785–90.
- Spencer KT, Flachskampf FA. Focused cardiac ultrasonography. JACC Cardiovasc Imaging. 2019;12:1243–1253.
- Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69:e27–e54.
- American College of Emergency Physians. Emergency ultrasound guidelines. Ann Emerg Med. 2009;53:550–70.
- Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the confirmation of endotracheal tube intubation: a systematic review and meta-analysis. Ann Emerg Med. 2018;72:627–636.
- Lanspa MJ, Grissom CK, Hirshberg EL, et al. Applying dynamic parameters to predict hemodynamic response to volume expansion in spontaneously breathing patients with septic shock. Shock. 2013;39:155–60.
- Airapetian N, Maizel J, Alyamani O, et al. Does inferior vena cava respiratory variability predict fluid responsiveness in spontaneously breathing patients? Crit Care. 2015;19:400.
- Muller L, Bobbia X, Toumi M, et al. Respiratory variations of inferior vena cava diameter to predict fluid responsiveness in spontaneously breathing patients with acute circulatory failure: need for a cautious use. Crit Care. 2012;16:R188.


 Issue PDF
Issue PDF