| Adapted from Special Feature on Pulse Oximeters: The invention that changed the paradigm of patient safety around the world. (LiSA (1340-8836) vol28 No3 Page237-308, 2021.03 (in Japanese)
Disclaimer: The information provided is for safety-related educational purposes only, and does not constitute medical or legal advice. Individual or group responses are only commentary, provided for purposes of education or discussion, and are neither statements of advice nor the opinions of APSF. It is not the intention of APSF to provide specific medical or legal advice or to endorse any specific views or recommendations in response to the inquiries posted. In no event shall APSF be responsible or liable, directly or indirectly, for any damage or loss caused or alleged to be caused by or in connection with the reliance on any such information. |
1. Introduction
Around 2007, Dr. Aoyagi once attended an in-company lab meeting with a newspaper clipping. The article reported a medical accident due to a missed alarm. At the very beginning, he insisted, “The performance of the device is the root cause. Performance improvement is essential in medical settings. We have to improve measurement technologies to reduce medical accidents.” He showed a strong sense of mission, saying, “fundamental improvement in the performance of pulse oximeters by constructing a theory not only allows a reduction in the burden on patients of blood collection, but also leads to the prevention of alarm-related accidents due to health care workers’ alarm fatigue 1). Furthermore, it widens the possibility of application contributing to health care, as a method of noninvasive and continuous measurement of light-absorbing materials in blood.”
Today, devices with closed loop control function have begun to be actively used, and the level of accuracy required for pulse oximeters is changing. From the beginning, Dr. Aoyagi had a clear vision that “the ultimate ideal of health care is automatic control of treatment,” and he worked actively to improve the performance. In this article, I introduce Dr. Aoyagi’s research on theory construction by multi-wavelength pulse oximetry.
2. Accuracy of Pulse Oximetry
First, I would like to explain the accuracy of pulse oximetry, which Dr. Aoyagi pursued throughout life. Although products currently on the market have an accuracy of approximately ± 2% SpO2 according to specifications, it should be noted that while two-thirds of the SpO2 values are within the range of accuracy specified (RMS: root mean square), one-third are outside the range, and that the range does not correspond to the 95% confidence interval. In addition, hypoxia exposure testing to verify the accuracy is performed under almost ideal conditions in healthy subjects, and various factors may further decrease accuracy in the actual clinical environment.
|
Column 1 The accuracy of pulse oximetry required by ISO (International Organization for Standardization) is defined as the RMS (concept close to residual standard deviation) of the difference between the pulse oximeter measurement and CO-oximeter measurement (as a reference) in human volunteers exposed to hypoxia. The accuracy acceptable by ISO is set at £4% for arterial oxygen saturation (SaO2) values of 70% to 100% (91% to 99% when the SaO2 was 95%). Dr. Aoyagi cited oxygen management in neonates as an example and set the goal of realizing true second-generation pulse oximetry with increased absolute accuracy, in order to reduce the patient burden by preventing retinopathy of prematurity and reducing renumber of blood collections. |
3. A Challenge to Fundamentally Improving the Accuracy
In this section, I introduce how Dr. Aoyagi worked on improving the accuracy of pulse oximeters by using multi-wavelengths. Two-wavelength pulse oximeters have already been described in various reports 3) and are omitted here.
Dr. Aoyagi recognized that there was room for improvement in the accuracy of pulse oximetry soon after the dissemination of two-wavelength pulse oximeters in Japan. A theory considering the effects of changes other than those in the arterial blood is required to improve the accuracy of pulse oximetry. Changes other than those in the arterial blood itself are caused by body motion and other factors, and he started a study based on the fundamental idea that the construction of this theory would lead to the elimination of body motion artifacts and provide a basis for significant future development.
In products of Masimo Corporation, which is a pioneer of algorithms with improved body motion-resistance performance, the most provable oxygen saturation is displayed as the SpO2 value by performing all calculations in the oxygen saturation range of 1% to 100%. Other companies have also adopted technologies to separate components corresponding to arterial oxygen saturation by extracting the characteristics of the pulse wave, but either technology involve assumptions. In contrast, Dr. Aoyagi tried to express all phenomena affecting the accuracy of pulse oximetry through mathematical formulae (i.e., to fix the theory). He tried to fundamentally improve the accuracy of pulse oximetry, with the belief that if all the ongoing phenomena can be explained, an accurate SpO2 value can be obtained.
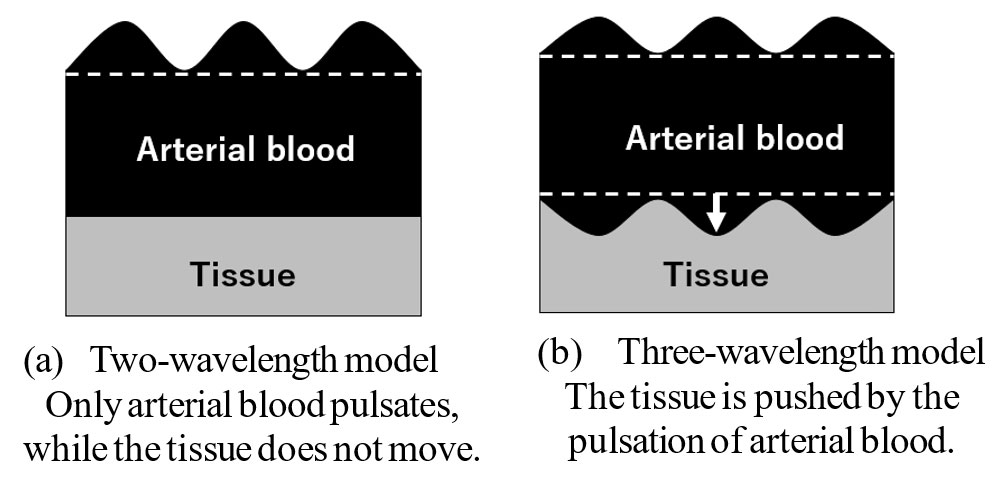
In the course of research, Dr. Aoyagi paid attention to the Lambert-Beer law, which is the basis for two-wavelength pulse oximetry. According to the law, the attenuation of light entering a medium (degree of optical attenuation) is proportional to the extinction coefficient, which indicates how much light a medium absorbs, and the thickness of the medium, if the medium is homogeneous. Oxygen saturation is supposed to be easily measured according to this law on the assumption that the pulsatile component of light transmission through living tissues is caused by light absorption of arterial blood (Figure 1 (a) two-wavelength model). However, practically, the degree of optical attenuation is not simply proportional to the extinction coefficient and the change in thickness, because it is affected by complex factors including not only light absorption, but also light scattering (Column 2). Since the theory has not been established, numerical values are displayed according to a look-up table based not on theoretical calculations, but on measured values obtained from subjects under severe hypoxic conditions. This method is invasive and reflects the reality in which there are no standardized calibration methods. Establishment of a theoretical formula will lead not only to improved accuracy and elimination of the effects of body motion, but also to the establishment of a standardized calibration method, which is not currently available.
Although light scattering was an unfamiliar field for Dr. Aoyagi, he worked energetically and tried to make improvements in the following order.
<1> To establish a theoretical formula for light absorption/scattering, including error factors 4)
(Schuster theory 5) was adopted for scattering.)
<2> To increase the number of light wavelengths and to equalize the number of equations for the attenuation ratio between two wavelengths (Φ) to the number of unknowns
<3> To set up simultaneous equations for Φ
<4> To obtain accurate SpO2 values from the simultaneous equations
| Column 2 Light scattering in vivoThere are two types of light scattering, as follows, regardless of the wavelength range.(1) Scattering depending on the wavelength, such as by the blue sky and glow of the sunset (a specific color is visible.)(2) Scattering independent of the wavelength, such as by a cloud or fog (looking white)In the wavelength range used in pulse oximeters, scattering (2) could be considered as being dominant in vivo 6). |
Consideration of the effects of tissues
Dr. Aoyagi first paid attention to non-blood living tissues as a significant factor other than arterial blood. When the effects of tissues are taken into account, arterial oxygen saturation and the effects of tissues are variable factors. Dr. Aoyagi obtained two attenuation ratios by measurements at three wavelengths to allow separation of the effects of changes in the arterial blood and changes in the tissues (Figure 1 (b) three-wavelength model). Here, I would like to explain how the effects of tissues emerge specifically. Attenuation changes by DAi at each wavelength li (i = 1,2,3) depending on the changes in the arterial oxygen saturation and tissue thickness, and Figure 2 shows the results of the simulations on the assumption of one of the two changing. The vertical axis represents the attenuation ratio of the two wavelengths used in conventional pulse oximeters DA2/DA3 (corresponding 1:1 to the SpO2 value), and the horizontal axis represents the attenuation ratio DA1/DA2 obtained using an additional wavelength (l1). The line passing through points A and B represents the change in the attenuation ratio when the tissue thickness does not change and only the oxygen saturation changes, while the line passing through points a and b represents the change in the attenuation ratio when the oxygen saturation remains constant and the tissue thickness changes. Although the oxygen saturation is different between points A and a, the two-wavelength system cannot distinguish the difference and displays the same oxygen saturation. It also cannot distinguish the difference between points B and b. Measurements at three wavelengths allow accurate determination of the oxygen saturation corrected for the effects of changes in the tissue thickness.

Figure 2: Simulations considering the effects of tissues
●: Changes in the attenuation ratio when tissue pulsation is absent and only oxygen saturation changes
□: Changes in the attenuation ratio when oxygen saturation is constant and the tissue thickness changes
At first, after his proposal of the theory in relation to tissues, this theory was not easily understood by people around him, due to the complicated behavior of light in vivo. However, Dr. Aoyagi confirmed his theory and explained it with conviction by the following procedure.
He investigated the effects of tissues by in vitro experiments using cuvettes (thin cells). Using a single-layer model in which only the arteries change (Figure 3 (a)) and a two-layer model in which tissues are simulated by a layer of cow’s milk (Figure 3 (b)), the attenuation ratio was measured when blood oxygen saturation in the cuvette was changed to compare the relationship between the oxygen saturation and the attenuation ratio with that in human subjects (Figure 4). The results showed that the relationship between the oxygen saturation and the attenuation ratio in the single-layer model was different from human data, that in the two-layer model was consistent with human data.
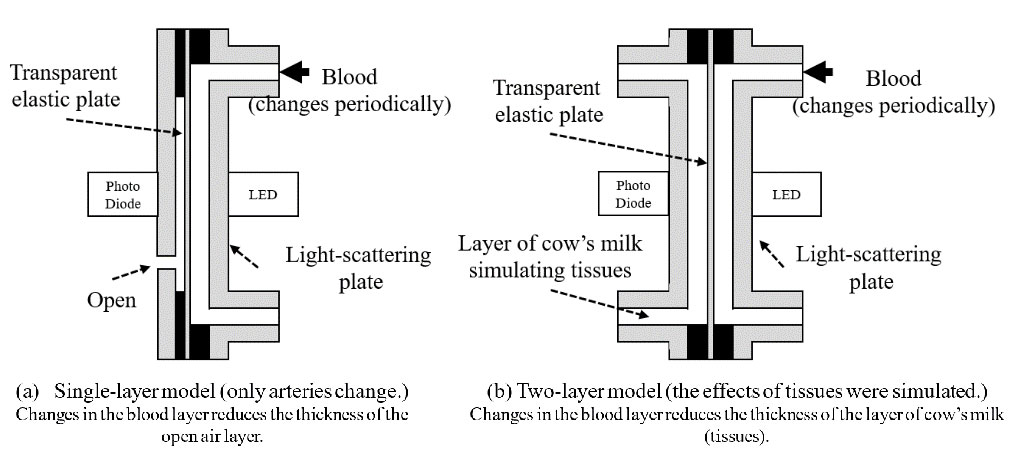
Figure 3: In vitro experimental models 7),8)
The thickness of the blood layer is changed periodically by changing the pressure of blood using a transparent elastic plate on one side of the blood layer.
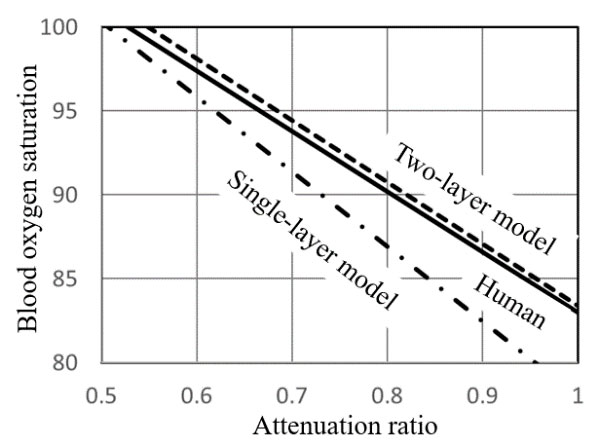
Figure 4: Comparison of measured values between the in vitro models and humans 7),8)
The measurement results in the two-layer model tended to be more closely similar to those in humans than those in the single-layer model.
He confirmed that the effects of tissues are a major error factor and concluded that the accuracy can be improved by wavelength multiplexing 7),8).
Consideration of the effects of veins
To further improve the accuracy, Dr. Aoyagi paid attention to the effects of venous blood in addition to those of tissues. Although it was difficult to construct a theory considering venous blood, he believed that the accuracy can be fundamentally improved by constructing a five-wavelength model considering the following 4 factors with optical effects.
Effects of arterial oxygen saturation
Effects of venous oxygen saturation
Effects of tissues
Effects of changes in the venous blood volume
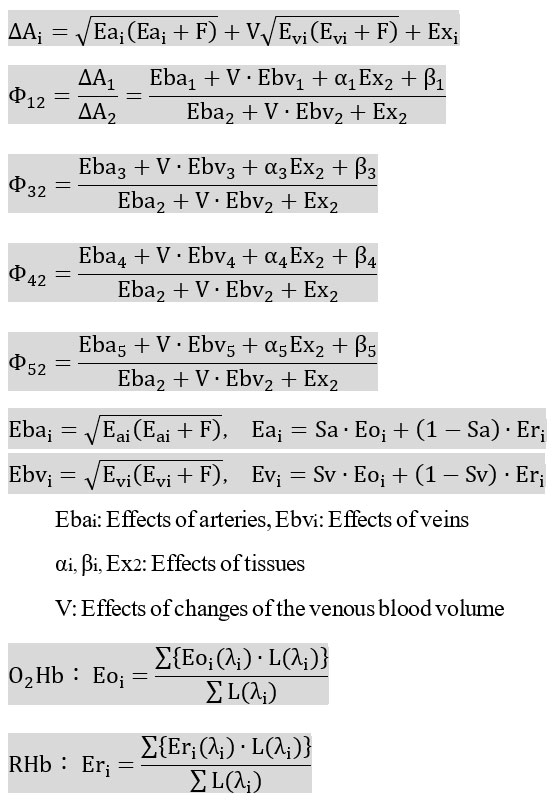
He thought that since there are 4 unknowns, if measurements are made at 5 wavelengths and simultaneous equations with 4 unknowns for the attenuation ratio Φ are set up, accurate SpO2 values could be obtained. Figure 5 shows simultaneous equations involving 5 wavelengths. Four unknowns are expressed in four dimensions, making it impossible to draw an illustration like Figure 2, and here I introduce only the equations. See the article by Dr. Aoyagi 9) for the detailed development of the multi-wavelength equations.
Figure 6 shows an example of a comparison between the two- and five-wavelength systems. Figure 6 (1) shows a comparison with the oxygen saturation measured in blood samples collected at rest, which confirms that the five-wavelength system improves the accuracy. Figure 6 (2) shows a comparison of the SpO2 values obtained with the two-wavelength system (b) and five-wavelength system (c) in experiments in which the oxygen saturation was changed by asking the subject to hold the breath and administration of 100% O2 by inhalation while body motion was added (I served as the subject of this study). Probes were attached to both hands, and body motion was added by asking the subject to rub a desk with one hand at random time intervals ranging from 0.5 to 2 seconds. SpO2 values obtained with the five-wavelength system were closer to those on the resting side as compared to the two-wavelength system. As expected at the start of the study, the five-wavelength system was confirmed not only to improve the accuracy, but also the body motion-resistance performance.
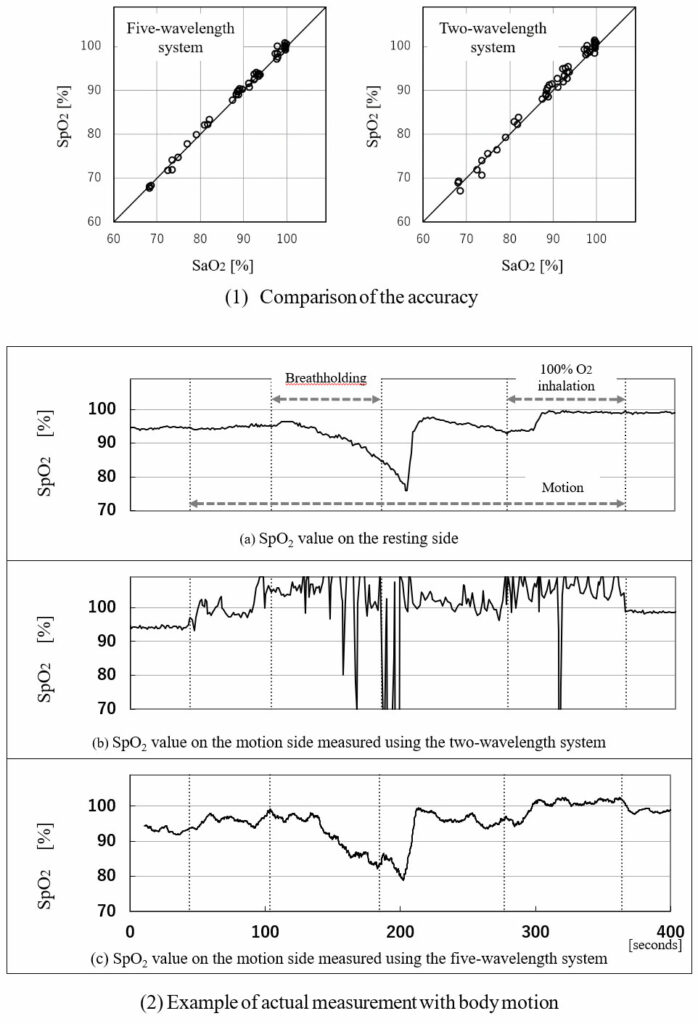
Figure 6: Comparison between the two- and five-wavelength systems
Example of actual measurement with body motion using the five-wavelength system
| Episode 1 Dr. Aoyagi used a method to stop the blood flow by binding his own finger for a long time, when conducting experiments to test the theory considering the effects of veins and tissues. He stopped blood flow by strongly binding the middle of a finger to which a probe was attached, measured the transmitted light while adding static pressure and pulsation to the probe attachment site using a small air-cuff. Meanwhile, blood oxygen saturation decreased spontaneously and a comparison with a hypothetical formula could be done 10).In these verification experiments, he found the optimal conditions after much trial and error. Since he wanted to measure up to extremely low oxygen saturation levels, he conducted the experiments while checking the time of finger binding, but he was completely absorbed in the experiments, saying “a little more, a little more.” For a while after that, he said with a smile that he still had no feeling in the numbed finger.Dr. Aoyagi always became a subject himself and devoted himself wholeheartedly to various pulse oximetry experiments. |
| Episode 2 IAMPOV*) was held in Japan (St. Luke’s International University, Tokyo) in 2015. A prototype of the five-wavelength pulse oximeter, which was introduced in this article, was placed in a device exhibition booth at the symposium, and visitors wore a probe to try the prototype. Soon after giving an invited talk, Dr. Aoyagi stood in the exhibition booth, wore a probe and gave a demonstration to let the visitors know better the performance of the five-wavelength pulse oximeter. To demonstrate that the pulse oximeter could indicate hypoxia even in the presence of body motion artifacts, Dr. Aoyagi, aged 79 years at that time, moved his hand vigorously while holding his breath to give an enthusiastic demonstration.*) International Symposium on Innovations and Applications of Monitoring Perfusion, Oxygenation and Ventilation |
4. Future issues/prospects
Construction of the theory of pulse oximetry considering the effects of tissues and veins has only been half accomplished. Recently, studies have been conducted on the adverse effects and efficacy of oxygen therapy using SpO2 values measured by pulse oximetry, but it has been reported that no conclusion has been reached on management with specified target SpO2 values 11). One of the reasons may be that the current accuracy of pulse oximetry does not meet the stringent requirements of clinical management. The projects introduced here are still in the research stage, and many problems remain to be resolved before the products are launched in the market. As a researcher working on improving the performance together with Dr. Aoyagi, I would like to follow in his footsteps and try to realize true second-generation pulse oximeters.
Dr. Aoyagi paid attention to pulse wave signals causing noise during measurement of the cardiac output by the dye dilution method and conceived the idea of pulse oximetry. If the theory of pulse oximetry is completed, signals causing noise could also be used as new information in the measurement of arterial oxygen saturation. At present, in perioperative systemic management, cardiac output and great vessel pressures are managed as representative values, and I think that development of a device that can noninvasively and continuously measure oxygen metabolism at the level of each organ/tissue, which is the ultimate indicator, will contribute to improving the outcome of patients or treatment.
Kazumasa Ito
Vital Sign Sensor Technology Development Division, Technology Development Operations,
NIHON KOHDEN CORPORATION
References
- Keith J Ruskin, James P Bliss, Alarm Fatigue and Patient Safety, APSF Newsletter, 2019; 34: 1-6
- ISO 80601-2-61(2018), Particular requirements for basic safety and essential performance of pulse oximeter equipment.
- Aoyagi T, Ukawa T. Principle and structure of pulse oximeter. Clinical Engineering 1996;7:102-110 (In Japanese)
- Aoyagi T. Theoretical and experimental study of optical attenuation of blood. Jpn J Med Elec Biol Eng 1992; 30, 1-7,
- Schustrer A. Radiation through a foggy atmosphere. Astrophys J 1905;21:1-22
- Nienle Bosschaart, Gerda J. Edelman, et al. A literature review and novel theoretical approach on the optical properties of whole blood. Lasers Med Sci.2014;29:453-479
- Aoyagi T, Miyasaka K:Pulse oximetry and its simulation.IEEE Tokyo Section 1990;29,184-186
- Aoyagi T, Fuse M, Miyasaka K. Basic Theory of Pulse Oximetry. Proceedings of the annual meeting of Japan Society of Technology in Anesthesia. 2010;13-20 (In Japanese)
- Aoyagi T, Miyasaka K, Machida K, et al. Multiwavelength Pulse Oximetry: Theory for the Future. Anesth Analg. 2007;105:S53-S58
- Aoayagi T, Fuse M, Kanemoto M, Xie C, Kobayashi N, Machida K, Miyasaka K. Theoretical and Experimental Study of Pulse Oximetry. Transactions of Japanese Society for Medical and Biological Engineering. 2012;50(3),299-307
- Kobayashi M. What about oxygen toxicity? (Target SpO2 values). The proceeding of the 47th Annual Meeting of the Japanese Society of Intensive Care Medicine. 2020; 97-100s (In Japanese)
| Read more articles from this special collection hosted by the APSF on Pulse Oximetry and the Legacy of Dr. Takuo Aoyagi. |
 Articles
Articles